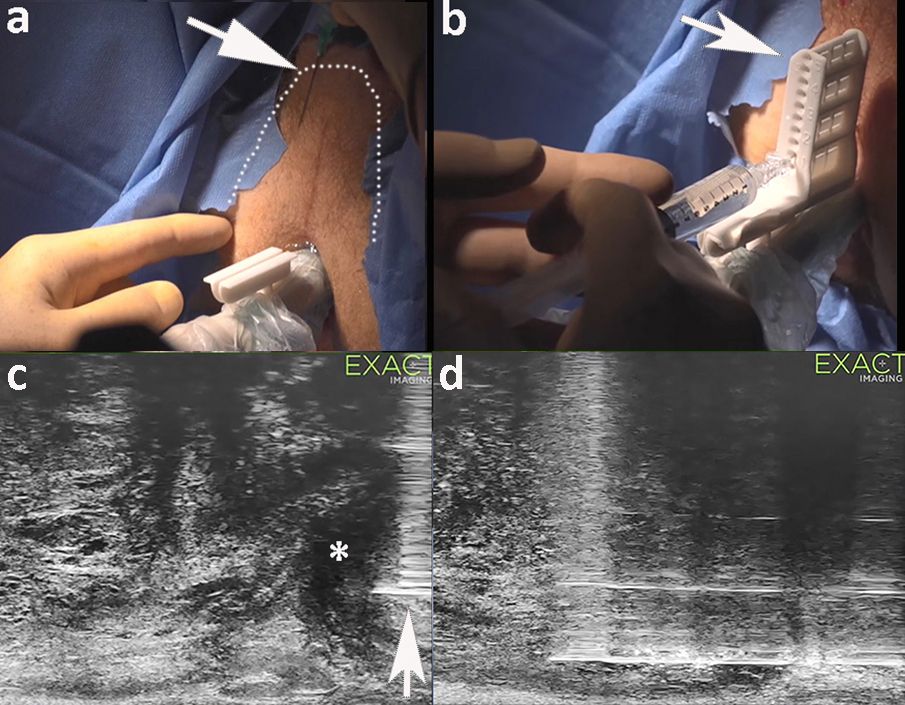
The meta-analysis does not mention that SB are positive, in at least half of the cases, in the target area, which questions the accuracy of TB, whatever the technique used. The imaging modality used to guide the needle pathway should ideally “see” the target at the time of biopsy. This is possible if real-time MRI guidance is used 2. It is also possible to use a conventional endorectal ultrasound probe equipped with a very high-quality B-mode. Which can localize PI-RADS 4-5 lesions originating in the peripheral zone (PZ) in 85-90% of cases, with the help, of a real time navigation system in selected cases3. It is even now possible to use a 29MHz linear array (Exact Imaging, Canada), also known as micro-ultrasound 4,5, which provides a spatial resolution never achieved until now for the prostate. When used as a second look modality (once the location of the lesion is known on MRI), this new technology may localize PZ lesions, whatever the PI-RADS category, and lower TZ tumors in virtually 100% of cases6. A navigation fusion system is available if the tumor is not well displayed on microUS (figure 1).
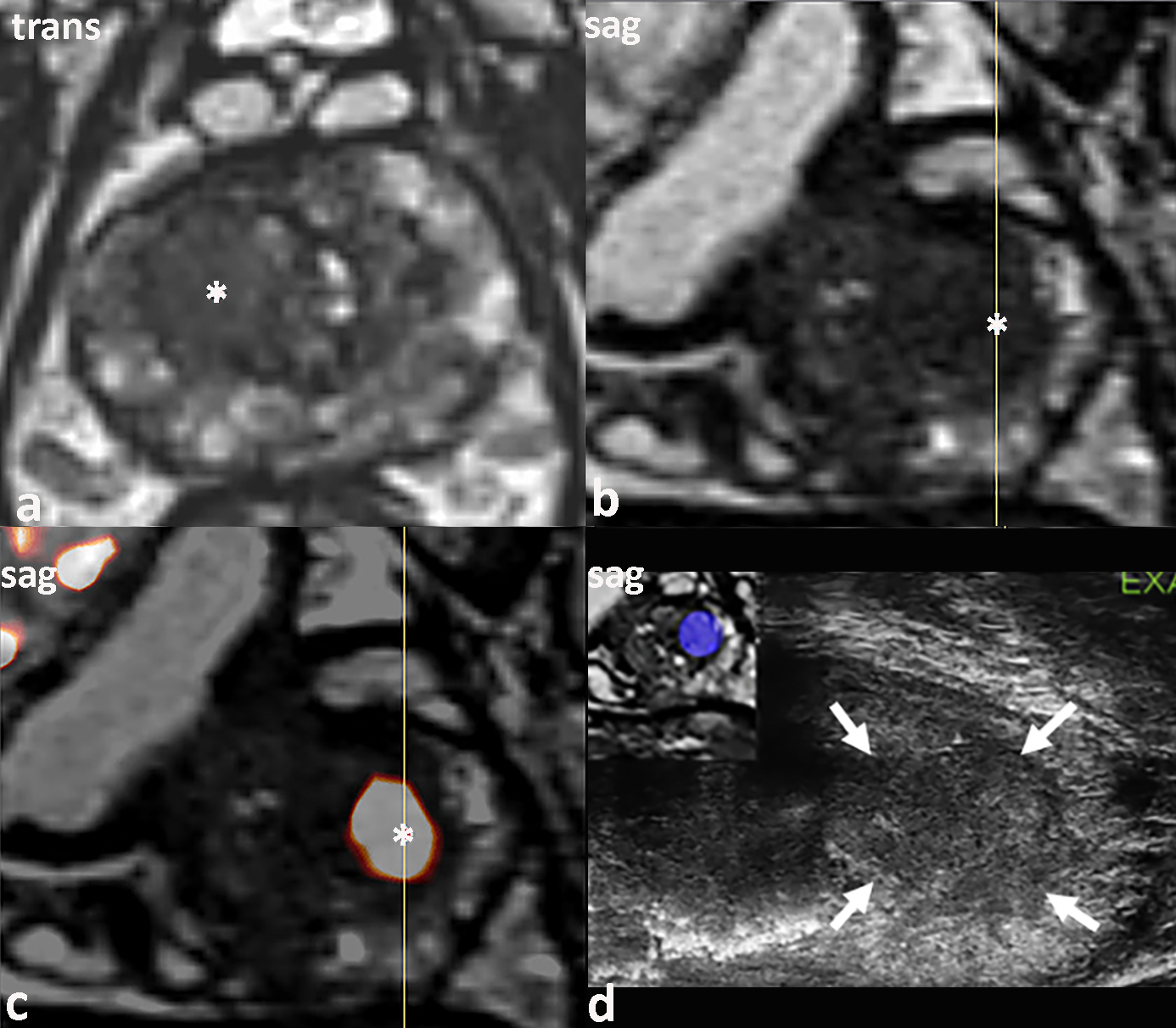
Figure 1 : 67 y/o man. PSA level : 7 ng/ml. Anterior TZ hyposignal (asterisk, a-b) with marked restricted diffusion (asterisk, c), visible on micro-ultrasound (white arrows, d) corresponding to a Gleason score 7 carcinoma on TRUS guided targeted biopsies. The blue tag on the left upper corner (d) is obtained by image fusion, which can be helpful if the anterior lesion is not well seen on micro ultra-sound.
There is actually more and more evidence that TB, whatever the technique used, should sample the target and its vicinity (“penumbra” 7) and SB far outside the lesion may be discarded.
It should also be noted that this meta-analysis is published at a time where the transrectal route is increasingly being questioned, given the septic risk it entails. The septic risk of the transrectal approach has been more and more often denounced these past years. More than one million prostate biopsies are performed in Europe and the United States every year. Fever or chills are observed in more than 10% of cases and a serious infection in 1-2% 8. One case of death has been reported in a Norwegian study 9, which warned that the resistance to antibiotics steadily increased and predicted that it will quadruple in the coming years. For some authors, the transrectal route is becoming untenable 9 and the routine use of rectal culture swabs prior to any transrectal biopsies is strongly encouraged to detect a quinolone-resistant germ 8.
The alternative is transperineal biopsies (TPB), initially done under general anesthesia to perform saturation biopsies. Now, local anesthesia is acceptable 1 (figure 2), with a conscious sedation in selected cases. The major advantage of TPB is the absence of infection, and the prophylaxis is done by IV injection of cepaholosporin 30 mn before the biopsy, avoiding the risks of the resistrance to quinolones.
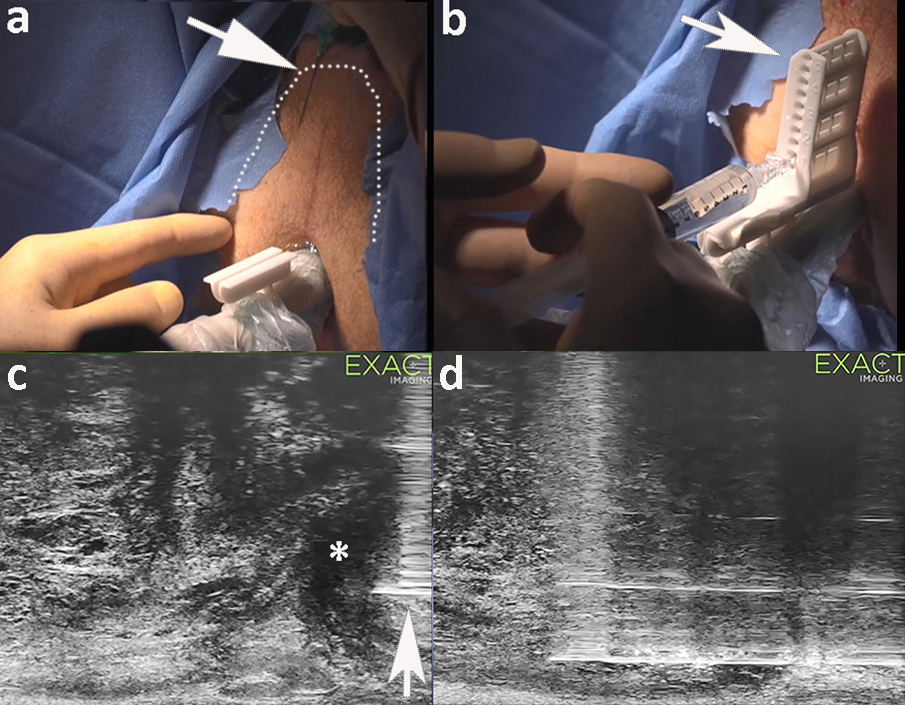
Figure 2 :Transperineal systematic biopsies in a 65 y/o man with a raising PSA. MRI showed no focal lesion. Local anesthesia (arrow, a),is first done subcutaneously covering a horseshoe shaped area (dotted line). The needle guide (arrow, b) is then positioned and used for the periprostatic anesthesia (arrow, c). Local spread of the lidocaine (asterisk, c) is followed in real-time. The needle biopsy (d) follows a cranio-caudal route when the biopsy device is activated, allowing for an optimal amount of PZ or TZ sampled tissue, when compared to a transrectal biopsy. A standard transperineal biopsy scheme includes 11 cores and can be increased to 20 cores if the TZ needs to be sampled.
It can be expected that the transperineal approach and a target+penumbra biopsy policy under local anesthesia will gain a more widespread acceptance in a short future.
References
1. Tu X, Liu Z, Chang T, et al: Transperineal Magnetic Resonance Imaging-Targeted Biopsy May Perform Better Than Transrectal Route in the Detection of Clinically Significant Prostate Cancer: Systematic Review and Meta-analysis. Clin Genitourin Cancer 17:e860-e870, 2019
2. Barral M, Lefevre A, Camparo P, et al: In-Bore Transrectal MRI-Guided Biopsy With Robotic Assistance in the Diagnosis of Prostate Cancer: An Analysis of 57 Patients. AJR Am J Roentgenol 213:171-179, 2019
3. van de Ven WJ, Venderink W, Sedelaar JP, et al: MR-targeted TRUS prostate biopsy using local reference augmentation: initial experience. Int Urol Nephrol 48:1037-45, 2016
4. Lughezzani G, Saita A, Lazzeri M, et al: Comparison of the Diagnostic Accuracy of Micro-ultrasound and Magnetic Resonance Imaging/Ultrasound Fusion Targeted Biopsies for the Diagnosis of Clinically Significant Prostate Cancer. Eur Urol Oncol 2:329-332, 2019
5. Ghai S, Eure G, Fradet V, et al: Assessing Cancer Risk on Novel 29 MHz Micro-Ultrasound Images of the Prostate: Creation of the Micro-Ultrasound Protocol for Prostate Risk Identification. J Urol 196:562-9, 2016
6. Cornud F, Lefevre A, Flam T, et al: MRI-directed high-frequency (29MhZ) TRUS-guided biopsies: initial results of a single-center study. Eur Radiol, 2020
7. Padhani AR, Weinreb J, Rosenkrantz AB, et al: Prostate Imaging-Reporting and Data System Steering Committee: PI-RADS v2 Status Update and Future Directions. Eur Urol 75:385-396, 2019
8. Thurtle D, Starling L, Leonard K, et al: Improving the safety and tolerability of local anaesthetic outpatient transperineal prostate biopsies: A pilot study of the CAMbridge PROstate Biopsy (CAMPROBE) method. J Clin Urol 11:192-199, 2018
9. Johansen TEB, Zahl PH, Baco E, et al: Antibiotic resistance, hospitalizations, and mortality related to prostate biopsy: first report from the Norwegian Patient Registry. World J Urol, 2019